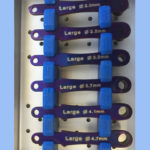
Here is a case of what I jokingly call “Suggested Surgery” as opposed to Guided Surgery. Patient came in with literally #24 in its entirety in his hand with his chief complaint of a broken tooth. He wanted to keep as many teeth as possible and realized that more teeth would be lost in the future. Scanned in both Galileos and CEREC. This is a great case for a Pilot Guide. As you may or may not know, Sirona does not make bone supported guides and as you can see from the PAs we have very uneven bone. We also have a fairly tight ridge bucco-ligually. So the plan is to place 3 3mm Legacy 3 implants and to do some bone re-contouring for a splinted 3 unit splinted FPD with some pink gingiva.

The whole concept of VIP (Virtually Integrated Patient) is pretty evident here. We fave the face scan as well as an optically scanned model. I do not need mounted study models as the case is “mounted” virtually and I can see we have a pretty strong Class III jaw relationship going on here. So I know not to plan my implant platforms lingual to the upper centrals, I want to actually be a bit buccal!

So we have a debatable treatment plan here. #23 and #25 are incredibly mobile with lots of granulation tissue. #26 is rock solid but radiographically looks not so good. I decided to keep it with the understanding that if in the 3 months of healing it loosens up, we take it out and cantilever off the 3 implants to #26. Patient wanted to keep as many teeth and was aware. 2.3mm Pilot guide, just to get spacing and angulation, but no real depth control. This is on purpose as we really do not know where the crest of the ridge will end up after we remove the granulation tissue and contour the bone.

Implants placed and pins checked at 2.3. Lots of really tenacious yucky tissue and uneven D1 bone. Used the Crestal Bone Drills up to a 2.8.

Implants in. Note how #24 deviated about the Symphasis. Thats the sucky thing about Pilots and why I call it Suggested Surgery, after the first drill you can still get some deviation. Will it matter? No. Will keep an eye on healing on the distal of #26 and watch for mobility.

Placed healing abutments. Normally I would apically place the flap but it became so “moth eaten” after getting rid of the inflammatory tissue that I just stitched it all together. At 3 months I will make a lingual incision horizontally and two releases and get that apical. Patient was cool with a flipper.

Metal Frame try in. We ended up taking out #26 as it was debatable if we wanted to keep it. So I figured we might as well remove it now and just cantilever. I guess I’m fickle like that ;} As you can see we have some good growth up over the healing abutments, so we made a crestal incision and brought the tissue buccal. Nice ginigval porcelain job by my man, Jack from Los Feliz dental lab